Help end the opioid crisis
Between January 2016 and September 2018, more than 10,300 Canadians died from an apparent opioid-related overdose. Many of those Canadians lived here in Vancouver, and some also had HIV/AIDS.
Here at the Dr. Peter Centre, we’ve cared for several people lost to this crisis. People with substance use disorders have always been a part of the community we care for, and the opioid crisis has made our work even more critical.
Doing what we can to stop the unexpected
As the death toll rose, the Dr. Peter Centre collaborated with the federal government and began working together on a new program that would take a non-judgmental harm reduction view to this serious public health problem.
"We know there is no silver bullet solution to this crisis, and the services and education these organizations offer are crucial. We must continue to work all together to save lives."
~ Ginette Petitpas Taylor, Federal Minister of Health, 2019
The result?
In 2019, Health Canada paved the way for the Dr. Peter Centre to launch a two-year pilot project to create and provide a safe and legal drug supply for those with opioid use disorder, and study how such a program works inside our holistic, integrated health care setting.
The intravenous agonist opioid therapy (iOAT) program allows individuals to receive prescribed hydromorphone (a medical-grade and safe painkiller) as an injectable opioid treatment twice daily. This assists with overdose prevention by providing an alternative to the tainted illicit drug supply.
FAQs
What is iOAT?
Injectable Opioid Agonist Treatment (iOAT) provides medically supervised pharmaceutical-grade opioids for injection
What is the evidence base?
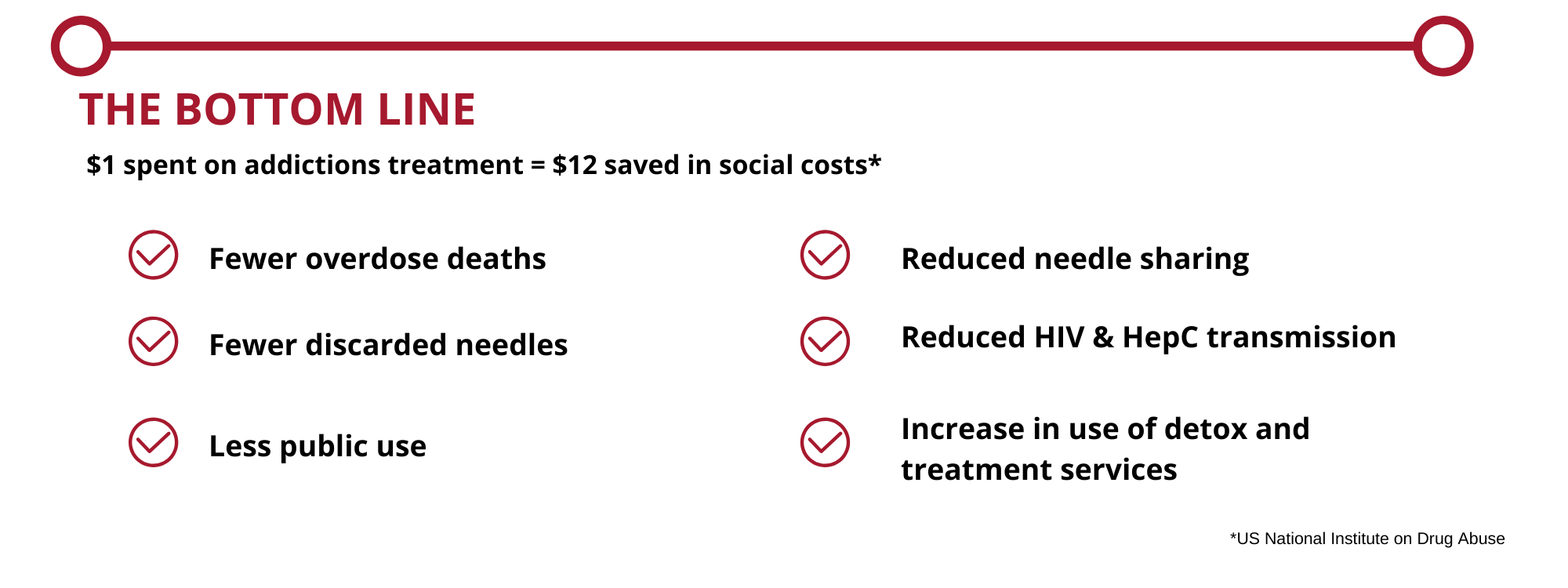
Reduced cost to society:
- Comprehensive iOAT care cost is $27,000 per year per patient vs. an estimated $45,000 per year per patient for an untreated opiate user (SALOME study)
- Involvement in criminal activity reduced from an average of 14 days/month to less than 4 days/month (SALOME study)
iOAT vs. methadone
- 67% reduction in illicit drug use or other illegal activity in iOAT group vs. 48% reduction in illicit drug use or illegal activity in methadone group (NAOMI trial)
- 88% retention rate in iOAT group at 12 months vs. 54% retention rate in methadone group at 12 months (NAOMI trial)
30-month program
Funded through Health Canada’s Substance Use & Addictions Program (SUAP)
Primary objectives
- implement a low-barrier pilot iOAT project in an integrated health care facility for people who use injection drugs and evaluate both the process and the effectiveness of integrating the treatment into this unique setting
- Determine the impact (if any) on drug-related harms including overdose, adherence to HIV treatment and overall health outcomes.
The aim is to contribute to the reduction and cessation of illicit street drugs by integrating participants into a health care setting where they can access both medical and psycho-social services and programs. In addition, the goal is to provide individuals with the tools and knowledge to make informed decisions about substance use and the benefits of iOAT compared to illicit drugs.
The lessons learned throughout this process will then be shared with up to 25 health service organizations nation-wide to so that similar projects can be successfully launched elsewhere.
We can't do this without you
This program couldn’t be possible without the support of Health Canada. And we still need you.
Our decades of experience working with people with HIV/AIDS taught us that treating the condition is only part of the solution. Equally important is treating the cause.
That’s why everyone in the iOAT program has access to our Day Health Program with twice-daily meals, and access to registered counsellors, including those certified in art, music and recreation therapy. With this program, there are now more to feed, more to care for.
Additionally, we want to provide a soft-landing as the program evolves from its pilot phase. We know people transition out of programs at their own pace, and so our focus is to ensure no one is left behind.
We need your support. Your contribution provides a solid foundation for those ready to take their first steps in building their own healthier future.
Help us do our part to end this crisis.
Program funding disclosure
This initiative has been made possible through a financial contribution from Health Canada’s Substance Use and Addictions Program. The views expressed herein do not necessarily represent the views of Health Canada.